Nursing Care Plan for Cirrhosis | Cirrhosis Overview
Cirrhosis of the liver Overview
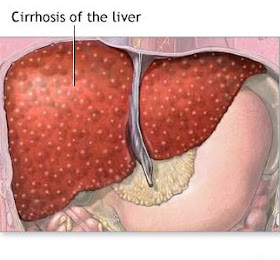
Cirrhosis is a chronic disease of the liver characterized by alteration in structure, degenerative changes and widespread destruction of hepatic cells, impairing cellular function and impeding blood flow through the liver.
Causes include malnutrition, inflammation (bacterial or viral), and poisons (e.g., alcohol, carbon tetrachloride, acetaminophen). Cirrhosis is the fourth leading cause of death in the United States among people ages 35 to 55 and represents a serious threat to long-term health.
Care Setting - Cirrhosis | Nursing Care Plan for Cirrhosis
- May be hospitalized on a medical unit during initial or recurrent acute episodes with potentially life-threatening complications. Otherwise, this condition is handled at the community level.
Related Concerns - Cirrhosis | Nursing Care Plan for Cirrhosis
- Alcohol: acute withdrawal
- Substance dependence/abuse rehabilitation
- Fluid and electrolyte imbalances
- Psychosocial aspects of care
- Renal dialysis
- Renal failure: acute
- Total nutritional support: parenteral/enteral feeding
- Upper gastrointestinal/esophageal bleeding
Here is an example of Nursing Care Plan for Cirrhosis.
Nursing Care Plan for Cirrhosis | Nursing Priorities; Discharge Goals
Nursing Priorities | Nursing Care Plan for Cirrhosis
- Maintain adequate nutrition.
- Prevent complications.
- Enhance self-concept, acceptance of situation.
- Provide information about disease process/prognosis, potential complications, and treatment needs.
Discharge Goals| Nursing Care Plan for Cirrhosis
- Nutritional intake adequate for individual needs.
- Complications prevented/minimized.
- Dealing effectively with current reality.
- Disease process, prognosis, potential complications, and therapeutic regimen understood.
- Plan in place to meet needs after discharge.
Nursing Care Plan for Cirrhosis | Nursing Diagnosis for Cirrhosis
Nursing Care Plan for Cirrhosis | Nursing Diagnosis for Cirrhosis; Desired Outcomes
Nursing Diagnosis for Cirrhosis: Nutrition: imbalanced, less than body requirements
May be related to
- Inadequate diet; inability to process/digest nutrients
- Anorexia, nausea/vomiting, indigestion, early satiety (ascites)
- Abnormal bowel function
- Possibly evidenced by
- Weight loss
- Changes in bowel sounds and function
- Poor muscle tone/wasting
- Imbalances in nutritional studies
Desired Outcomes/Evaluation Criteria | Nursing Care Plan for Cirrhosis
Patient Will:
Nutritional Status (NOC)
- Demonstrate progressive weight gain toward goal with patient-appropriate normalization of laboratory values.
- Experience no further signs of malnutrition.
Nursing Care Plan for Cirrhosis | Nursing Interventions for Cirrhosis
Nursing Care Plan for Cirrhosis | Nursing Interventions for Cirrhosis and Rationale;
Nursing Interventions for Cirrhosis and Rationale
Nutrition Therapy (NIC)
Nursing Interventions for Cirrhosis (Independent) | Nursing Care Plan for Cirrhosis
- Measure dietary intake by calorie count. Rationale: Provides information about intake, needs/deficiencies.
- Weigh as indicated. Compare changes in fluid status, recent weight history, skinfold measurements. Rationale: It may be difficult to use weight as a direct indicator of nutritional status in view of edema/ascites. Skinfold measurements are useful in assessing changes in muscle mass and subcutaneous fat reserves.
- Assist/encourage patient to eat; explain reasons for the types of diet. Feed patient if tiring easily, or have SO assist patient. Consider preferences in food choices. Rationale: Improved nutrition/diet is vital to recovery. Patient may eat better if family is involved and preferred foods are included as much as possible.
- Encourage patient to eat all meals/supplementary feedings. Rationale: Patient may pick at food or eat only a few bites because of loss of interest in food or because of nausea, generalized weakness, malaise.
- Recommend/provide small, frequent meals. Rationale: Poor tolerance to larger meals may be due to increased intra-abdominal pressure/ascites.
- Provide salt substitutes, if allowed; avoid those containing ammonium. Rationale: Salt substitutes enhance the flavor of food and aid in increasing appetite; ammonia potentiates risk of encephalopathy.
Nutrition Therapy (NIC)
Nursing Interventions for Cirrhosis (Independent) - continuation| Nursing Care Plan for Cirrhosis
- Restrict intake of caffeine, gas-producing or spicy and excessively hot or cold foods. Rationale: Aids in reducing gastric irritation/diarrhea and abdominal discomfort that may impair oral intake/digestion.
- Suggest soft foods, avoiding roughage if indicated. Rationale: Hemorrhage from esophageal varices may occur in advanced cirrhosis.
- Encourage frequent mouth care, especially before meals. Rationale: Patient is prone to sore and/or bleeding gums and bad taste in mouth, which contributes to anorexia.
- Promote undisturbed rest periods, especially before meals. Rationale: Conserving energy reduces metabolic demands on the liver and promotes cellular regeneration.
- Recommend cessation of smoking. Rationale: Reduces excessive gastric stimulation and risk of irritation/bleeding.
Nutrition Therapy (NIC)
Nursing Interventions for Cirrhosis (Collaborative) | Nursing Care Plan for Cirrhosis
- Monitor laboratory studies, e.g., serum glucose, prealbumin/albumin, total protein, ammonia. Rationale: Glucose may be decreased because of impaired glycogenesis, depleted glycogen stores, or inadequate intake. Protein may be low because of impaired metabolism, decreased hepatic synthesis, or loss into peritoneal cavity (ascites). Elevation of ammonia level may require restriction of protein intake to prevent serious complications.
- Maintain NPO status when indicated. Rationale: Initially, GI rest may be required in acutely ill patients to reduce demands on the liver and production of ammonia/urea in the GI tract.
Nutrition Therapy (NIC)
Nursing Interventions for Cirrhosis (Collaborative) - continuation | Nursing Care Plan for Cirrhosis
- Consult with dietitian to provide diet that is high in calories and simple carbohydrates, low in fat, and moderate to high in protein; limit sodium and fluid as necessary. Provide liquid supplements as indicated. Rationale:High-calorie foods are desired inasmuch as patient intake is usually limited. Carbohydrates supply readily available energy. Fats are poorly absorbed because of liver dysfunction and may contribute to abdominal discomfort. Proteins are needed to improve serum protein levels to reduce edema and to promote liver cell regeneration. Note: Protein and foods high in ammonia (e.g., gelatin) are restricted if ammonia level is elevated or if patient has clinical signs of hepatic encephalopathy. In addition, these individuals may tolerate vegetable protein better than meat protein.
- Provide tube feedings, TPN, lipids if indicated. Rationale: May be required to supplement diet or to provide nutrients when patient is too nauseated or anorexic to eat or when esophageal varices interfere with oral intake.
Nutrition Therapy (NIC)
Nursing Interventions for Cirrhosis (Collaborative) - continuation | Nursing Care Plan for Cirrhosis
- Administer medications as indicated, e.g.:
- Vitamin supplements, thiamin, iron, folic acid; Rationale: Patient may be vitamin-deficient because of previous poor diet. Also, the injured liver is unable to store vitamins A, B complex, D, and K. Anemia due to iron and folic acid deficiencies may also exist.
- Zinc; Rationale: Enhances sense of taste/smell, which may stimulate appetite.
- Digestive enzymes, e.g., pancrelipase (Viokase); Rationale: Promotes digestion of fats and may reduce steatorrhea/diarrhea.
- Antiemetics, e.g., trimethobenzamide (Tigan). Rationale: Used with caution to reduce nausea/vomiting and increase oral intake.
This is a sample of Nursing Care Plan for Cirrhosis.